A Practical Guide to Reducing Inflammation in Joints

When it comes to reducing inflammation in your joints, you need to think bigger than just masking the pain. A truly effective approach is about playing both offence and defence—using immediate relief tactics like topical analgesics for flare-ups while building a long-term lifestyle with an anti-inflammatory diet and smart exercise.
The goal is simple: manage the discomfort right now while tackling the biological triggers that cause it in the first place.
Understanding Why Your Joints Are Inflamed

Before we can fix the problem, we need to understand what's actually happening inside the joint. At its core, joint inflammation is your body's natural defence system kicking into gear in response to an injury, infection, or a chronic condition.
Think of it as your body's emergency response team. When it senses a threat, it floods the area with immune cells and other inflammatory substances. This is what causes those tell-tale signs: pain, swelling, redness, and stiffness.
This process is incredibly helpful when you've just sprained your ankle, but it becomes a major issue when it sticks around. With conditions like arthritis, the immune system gets its wires crossed and starts attacking healthy joint tissue. This creates a constant state of inflammation that can slowly wear away cartilage and bone.
The Scope of Joint Inflammation in Canada
If you're dealing with angry, inflamed joints, you are definitely not alone. It's a massive public health issue here in Canada, affecting a staggering 6 million adults—that's one in five people.
The numbers vary quite a bit across the country. Back in 2007-2008, Nova Scotia reported a crude prevalence of 23%, while Quebec was at just 12%. These statistics paint a clear picture: we need effective, accessible strategies for reducing joint inflammation, especially since projections show the number of affected Canadians could hit 9 million by 2045.
And it’s not just about chronic diseases. Even a temporary illness can set off a chain reaction. You’ve probably felt this yourself—that achy, sore feeling when you're sick. Understanding why your joints and muscles hurt when you have the flu shows just how much systemic inflammation can impact your entire body.
A Holistic View on Joint Care
To manage joint inflammation for good, you need a two-pronged strategy: immediate relief to handle the pain now and long-term prevention to stop it from coming back. It’s less about reacting to flare-ups and more about proactively building a lifestyle that keeps inflammation in check.
This means looking at your daily habits through an anti-inflammatory lens. The key pieces of the puzzle are:
- Dietary Choices: Prioritizing foods that actively fight inflammation while steering clear of the ones that fuel it.
- Mindful Movement: Sticking to gentle, low-impact exercises that strengthen the muscles supporting your joints without adding extra stress.
- Targeted Relief: Using non-prescription options, like topical analgesics, for quick, on-the-spot support when a flare-up hits.
By weaving these elements together, you build a sustainable framework for better joint health. It's about empowering yourself with a complete toolkit that addresses both the symptoms and the root causes of your discomfort.
This approach flips the script, turning joint care from a chore into a proactive, daily practice. For a deeper dive into inflammation and how to manage it, this comprehensive guide on reducing inflammation is a great resource. It's all about making small, consistent changes that add up to significant, lasting relief.
How to Get Immediate Relief from Joint Pain

When a joint inflammation flare-up hits, the pain can be sharp and completely derail your day. Long-term strategies are important, but in that moment, your only goal is finding relief—fast. Luckily, there are a few tried-and-true methods that can help calm angry joints and get you back on your feet.
The classic R.I.C.E. method (Rest, Ice, Compression, and Elevation) is a go-to for a reason. But how you do it matters. When you grab an ice pack, for example, don't just slap it on your skin. Always wrap it in a thin towel first and apply it for 15-20 minute intervals. This helps reduce swelling without risking an ice burn.
Resting the joint doesn't mean you have to be completely still, either. If your knee is throbbing, propping your leg up while you work at your desk counts. For extra stability when you need to get around, some people find that assistive devices like walkers and rollators can take a lot of strain off an inflamed joint. These are simple but powerful first steps.
Harnessing the Power of Topical Analgesics
For targeted relief right where it hurts, a good topical analgesic is a must-have. Unlike pills that have to work their way through your entire system, a topical treatment is applied directly to the source of the pain. This means the active ingredients get to work almost immediately.
Picture a runner with a sore knee after a long run, or maybe you've got a stiff neck from sitting at a computer all day. A quick spray or roll-on can deliver on-the-spot relief without missing a beat.
The ingredients in these products are what make them so effective. You’ll often find:
- Menthol: Creates a cooling sensation that works by activating certain sensory receptors, which helps temporarily block pain signals from reaching your brain.
- Methyl Salicylate: Provides a warming effect that helps boost blood flow to the area, which can relax tight muscles and soothe aching joints.
These sensations are known as counterirritants. They essentially create a new feeling that distracts your brain from the underlying pain, overriding the discomfort from the inflamed joint. If you're weighing your options, understanding the benefits of a topical pain reliever versus an oral pain reliever can help you make an informed choice.
The Bigger Picture of Immediate Relief
Finding accessible, immediate ways to manage joint inflammation is a major concern in Canada. The prevalence of arthritis continues to rise, contributing to an estimated $33 billion annual cost in healthcare and lost productivity. That staggering number really drives home why effective, over-the-counter solutions are so vital for both individuals and the healthcare system.
Topicals provide a practical, effective way to manage flare-ups, allowing you to stay active and engaged in daily life. This immediate control is empowering, turning a moment of pain into a manageable situation.
Ultimately, getting fast relief comes down to having a smart toolkit ready to go. When you combine the foundational principles of R.I.C.E. with the targeted power of a high-quality topical analgesic, you have an effective response for the moment pain strikes. It’s a critical first step in your broader strategy for long-term joint health.
Fueling Your Body with an Anti-Inflammatory Diet
While topical relief is great for managing flare-ups, the food you eat every single day plays a massive role in your long-term game plan for reducing joint inflammation. Think of your diet as the foundation of your joint health. What you build on top matters, but a shaky foundation will always lead to trouble.
Switching to an anti-inflammatory eating style isn't about harsh restrictions. It's about consciously adding vibrant, powerful foods that actively work to calm your system down.
Every meal is a chance to either fuel inflammation or fight it. A breakfast of a white bagel with cream cheese, for instance, can cause a spike in blood sugar—a well-known trigger for inflammatory responses. Swap that for a bowl of oatmeal topped with blueberries and walnuts, and you’ve completely changed the game. That simple switch gives you fibre to help lower inflammatory markers, plus a dose of antioxidants and healthy fats to protect your joints.
It’s these small, consistent choices that add up to significant, lasting change.
Building Your Anti-Inflammatory Plate
Creating meals that fight back against inflammation is simpler than you might think. The key is to zero in on whole, unprocessed foods that are packed with nutrients. This just means filling your shopping basket with colourful fruits and vegetables, lean proteins, and healthy fats.
A fantastic starting point is getting more omega-3 fatty acids into your diet. They’re famous for their potent anti-inflammatory properties, working behind the scenes to interfere with the body's inflammatory pathways and helping to ease joint stiffness and pain. You don't need to overhaul everything overnight; just aim for two servings of fatty fish each week to start.
Here are some anti-inflammatory powerhouses to add to your grocery list:
- Fatty Fish: Salmon, mackerel, and sardines are top-tier sources of omega-3s.
- Leafy Greens: Spinach, kale, and other dark greens are loaded with vitamins and antioxidants that act like bodyguards for your joints.
- Berries: Blueberries, strawberries, and raspberries contain anthocyanins, which are powerful antioxidants that battle inflammation.
- Nuts and Seeds: Walnuts and flaxseeds are excellent plant-based sources of omega-3s.
- Olive Oil: Extra virgin olive oil is rich in healthy fats that can help bring down inflammation levels.
Think of these foods as your internal defence team. The more you include them in your diet, the better equipped your body is to manage and reduce chronic joint inflammation naturally.
This approach really puts you in the driver’s seat, turning your kitchen into a powerful tool for better joint health.
Foods That Fan the Flames of Inflammation
Just as some foods can calm inflammation, others can make it much worse. Figuring out what these culprits are and limiting them is a critical step in managing your joint pain. The main offenders are usually highly processed foods loaded with sugar, unhealthy fats, and refined carbohydrates.
These types of foods can trigger the release of inflammatory messengers in the body, creating a vicious cycle of pain and stiffness. For instance, sugary drinks like soda and many packaged snacks can lead to a sharp spike in blood sugar, which directly promotes an inflammatory response.
Likewise, foods high in saturated and trans fats—think red meat and a lot of fried foods—are known to fuel inflammation. The goal isn’t to cut these things out completely, but to be mindful of how often you're eating them. Making conscious swaps where you can will make a world of difference.
Simple Anti-Inflammatory Food Swaps for Everyday Meals
Changing your diet can feel like a huge task, but the secret is to focus on simple, practical swaps. You don't need a perfect diet; you just need a better one. Remember, it's all about progress, not perfection.
The table below offers some easy ideas to replace common pro-inflammatory foods with anti-inflammatory alternatives that are just as satisfying.
| Instead Of This (Pro-Inflammatory) | Try This (Anti-Inflammatory) | Why It Helps |
|---|---|---|
| White Bread or a Bagel | Whole-Grain Toast or Oatmeal | Provides fibre, which helps lower C-reactive protein (CRP), a key inflammation marker. |
| Sugary Cereal | Greek Yogurt with Berries and Nuts | Delivers protein, antioxidants, and healthy fats without the inflammatory sugar spike. |
| Processed Snack Foods (Chips, Cookies) | A Handful of Almonds or an Apple | Replaces empty calories and unhealthy fats with fibre, vitamins, and anti-inflammatory fats. |
| Red Meat (like Steak or Burgers) | Fatty Fish (like Salmon) | Swaps pro-inflammatory saturated fats for powerful anti-inflammatory omega-3 fatty acids. |
| Vegetable Oil for Cooking | Extra Virgin Olive Oil | Contains oleocanthal, a compound with effects similar to non-steroidal anti-inflammatory drugs. |
Each one of these changes might seem small on its own, but when you put them together, they create a powerful cumulative effect. By consistently choosing foods that nourish your body and calm inflammation, you build a much more resilient foundation for healthier, more comfortable joints.
Smart Exercise for Stronger and Healthier Joints
When your joints are screaming in pain, the last thing on your mind is probably movement. It sounds backward, but gentle, consistent exercise is one of the most powerful long-term tools for getting inflammation under control. The trick is to find that sweet spot—strengthening the muscles that support your joints without pushing them past their limits and triggering more pain.
Think of the muscles around your knee or shoulder as a natural brace. The stronger and more flexible they are, the less stress the joint itself has to take on. Letting them get weak from inactivity? That just leaves your joints more vulnerable and can make inflammation and pain even worse.
The goal isn't to run a marathon next week. It's about weaving low-impact activities into your day that build strength and mobility without jarring sensitive joints.
Choosing the Right Low-Impact Activities
Half the battle is finding an activity you actually like because consistency is where the real results are. Low-impact exercises are perfect because they get your heart rate up and build muscle without pounding on your joints.
Here are a few great places to start:
- Swimming or Water Aerobics: The water’s buoyancy supports your body weight, taking almost all the pressure off your joints. It's an incredible environment for gentle resistance training.
- Cycling: Whether it's on a stationary bike or a flat trail outdoors, cycling is a fantastic way to build up your leg muscles without the high impact of running. Just make sure your bike is fitted properly to avoid putting extra strain on your knees.
- Tai Chi: This gentle practice combines slow, flowing movements with deep breathing. It’s known to improve balance, flexibility, and strength while also dialing down stress—which can be a major inflammation trigger on its own.
Remember, the best exercise is the one you’ll actually do. Start small, maybe just 10-15 minutes a day, and slowly add more time as you feel stronger and more comfortable.
This gradual ramp-up helps your body adapt and avoids the kind of overexertion that can send you right back to square one with a painful flare-up.
Creating a Complete Cycle of Joint Care
A smart exercise routine is more than just the movement itself. It’s also about what you do before and after to get your body ready and help it recover. When you create this complete cycle of care, you make it much easier to stay active while keeping inflammation in check.
This is where a proactive approach with topical analgesics can be a game-changer. For instance, if your knees are always stiff before a morning walk, applying a warming topical stick beforehand can help boost blood flow and loosen things up. That simple prep step makes those first few minutes of movement so much more comfortable.
After you're done, a cooling roll-on can be your new best friend. The cooling sensation helps soothe any post-exercise soreness and calms down potential inflammation before it gets a chance to flare up. This pre- and post-activity routine can turn exercise from something you dread into a manageable—and even enjoyable—part of your day.
This flowchart shows a simple but effective way to apply the same logic to your diet, swapping out inflammatory triggers for healthier, antioxidant-rich foods.
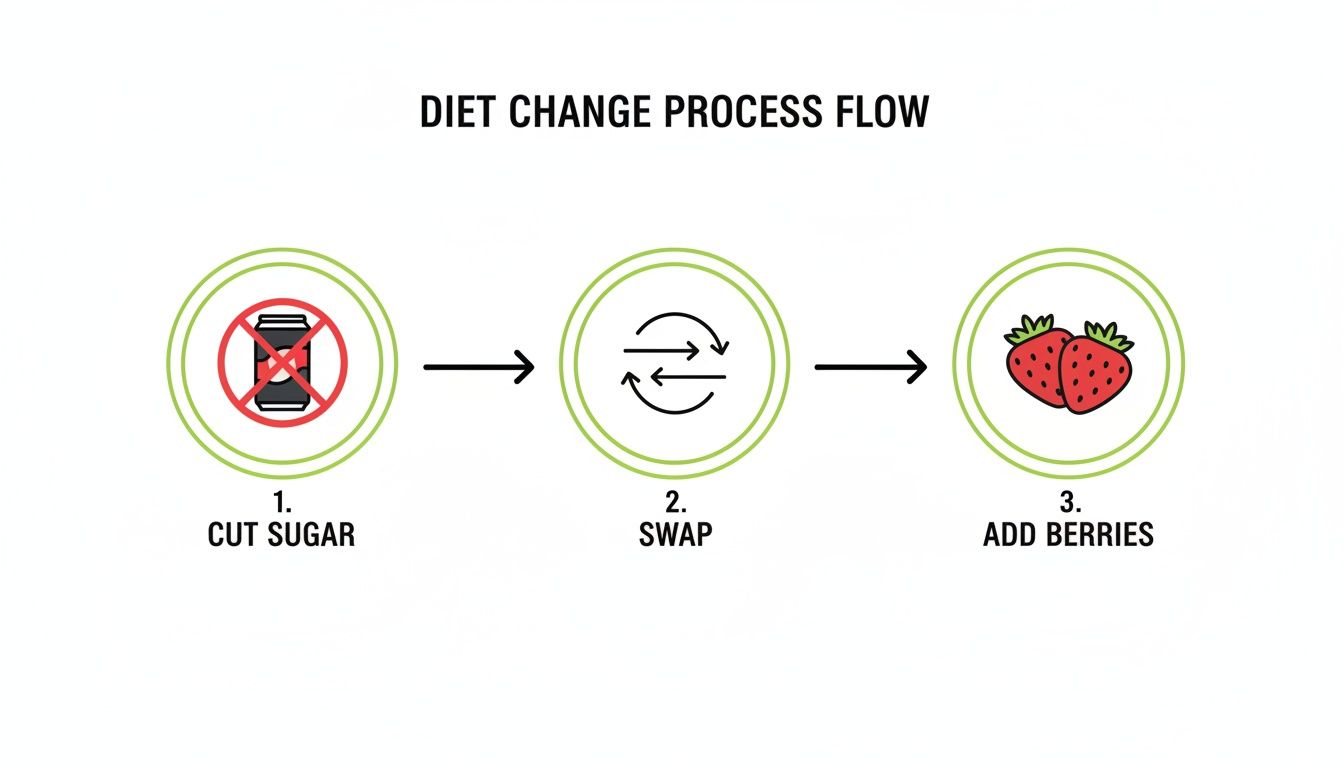
It’s a great reminder that small, strategic swaps in your daily habits—whether it’s what you eat or how you move—can add up to a huge impact on managing inflammation.
Strength, Flexibility, and Core Stability
While low-impact cardio is fantastic, a truly solid routine should also include work on strength, flexibility, and core stability. Your core muscles are the foundation for every move you make. A strong core helps you maintain proper posture and alignment, which takes a ton of unnecessary strain off joints all the way from your spine down to your ankles. Our guide on exercise for core stability has some excellent starting points.
Flexibility is just as critical. Gentle stretching keeps your range of motion from shrinking and prevents that locked-up feeling. Try to add a few simple stretches after your workout when your muscles are warm and more willing to cooperate.
For many Canadians, conditions like rheumatoid arthritis (RA) make this focus on smart exercise a necessity. RA affects about 1% of Canadians, and women are three times more likely to be diagnosed. Because it can cause chronic joint damage if not managed well, pairing gentle movement with targeted relief from products like MEDISTIK can be a powerful first line of defence.
By combining low-impact cardio with strength and flexibility work—and supporting it all with a smart pre-and-post-activity care routine—you build a powerful defence against joint inflammation. This approach helps you move with more confidence and less pain, turning exercise back into something that makes you feel good.
Knowing When to See a Healthcare Professional
Self-care strategies are fantastic for managing the day-to-day aches of joint inflammation, but they do have their limits. Knowing the difference between a manageable flare-up and a serious issue is a critical skill for protecting your long-term joint health. It’s all about being a confident and informed advocate for your own well-being.
Sometimes, joint pain isn't just a sign of overuse or a minor strain; it can be a warning signal from your body that something more significant is going on. Ignoring these red flags can delay diagnosis and treatment, potentially allowing more serious joint damage to occur.
Recognizing Red Flag Symptoms
While mild to moderate stiffness and aches can often be managed at home, certain symptoms demand immediate professional attention. These aren't the kinds of issues to "wait and see" about. If you experience any of the following, it’s time to book an appointment with a healthcare professional.
Think of these as non-negotiable signs that your body needs expert help:
- Sudden and Severe Pain or Swelling: If a joint suddenly becomes intensely painful and swells up without a clear cause, it could signal an infection or a serious inflammatory event.
- Fever Accompanied by Joint Pain: When you have a fever alongside joint pain, it may indicate a systemic infection or a significant autoimmune flare-up that needs medical evaluation.
- Inability to Bear Weight: If a joint in your leg or foot becomes so painful you can't put any weight on it, this is a clear sign that something is seriously wrong.
- Visible Deformity or Immobility: Any obvious change in the shape of a joint or a sudden loss of its normal range of motion warrants a professional diagnosis.
Trust your instincts. If the pain feels different, more severe, or is accompanied by other unusual symptoms, seeking medical advice is always the right decision. This proactive step ensures you get an accurate diagnosis and a treatment plan tailored to your specific needs.
Who to See for Joint Inflammation
Navigating the healthcare system can feel a bit overwhelming, but knowing which professional to turn to can make the process much smoother. Your journey toward a diagnosis and an effective treatment plan will likely start with your primary care provider.
Your Family Doctor
Your family doctor is your first and most important point of contact. They can perform an initial examination, order preliminary tests like blood work or X-rays, and provide a referral to a specialist if needed. Think of them as the coordinator of your care team.
Physiotherapist
For issues related to movement, strength, and mobility, a physiotherapist is an invaluable resource. They can design a personalized exercise program focused on strengthening the muscles around your joints, improving flexibility, and reducing pain through targeted, safe movements.
Rheumatologist
If your doctor suspects an autoimmune condition like rheumatoid arthritis, they will refer you to a rheumatologist. These specialists are the experts in diagnosing and treating inflammatory diseases that affect the musculoskeletal system.
Preparing for Your Appointment
To get the most out of your visit, a little preparation goes a long way. Before you go, take some time to really think about your symptoms in detail. This will help your healthcare provider get a clear picture of what's been happening.
Be ready to discuss:
- When the pain started and what you were doing at the time.
- What seems to make the pain better or worse.
- Any other symptoms you've experienced, even if they seem unrelated.
- A list of all medications and supplements you are currently taking.
Being prepared helps ensure you receive a comprehensive evaluation and a treatment plan that addresses the root cause of your joint inflammation, setting you on the right path to effective, long-term relief.
Quick Answers to Your Joint Health Questions
When it comes to managing joint inflammation, you've got the big picture—diet, exercise, and immediate relief. But how does that all fit into your actual, day-to-day life? It’s one thing to know what to do, but another thing entirely to know how.
Let's dig into some of the most common questions I hear from people. We’ll get straight to the practical, real-world answers you need to manage your joint health with confidence.
How Long Does It Take to See Results from Diet Changes?
This is probably the number one question people ask, and the honest answer is, it depends. An anti-inflammatory diet isn't like popping a painkiller; you're playing the long game here, fundamentally changing your body's internal environment. That takes time.
Most people start noticing small shifts within a few weeks to a couple of months—maybe a little less stiffness when you wake up or just a general decrease in that constant, dull ache. The real secret is consistency over perfection. Every anti-inflammatory meal you eat is a win, building up a positive effect over time.
Can Exercise Make My Joint Inflammation Worse?
It’s a totally valid fear. When everything hurts, the last thing you want to do is move and make it worse. And yes, the wrong kind of exercise, like high-impact moves during a flare-up, can definitely set you back. But the right kind of movement is absolutely crucial for healthy joints.
The trick is to listen to your body and stick to low-impact activities.
- Smart Choices: Think swimming, gentle cycling, or tai chi. These build muscle to support your joints without hammering them.
- Red Flags: Sharp, stabbing pain is your body’s signal to stop. Right now. Don't push through it.
- The Day After: A bit of muscle soreness is fine, but if your joint pain is noticeably worse the next day, you likely overdid it. Scale it back.
A good rule of thumb is to start slow and build up gradually. Gentle, consistent movement helps lubricate your joints and actually reduces inflammation, making it one of your most powerful tools.
Are Supplements Actually Effective for Joint Inflammation?
The supplement aisle can be overwhelming, but there are a few that have solid evidence behind them for supporting joint health. They aren't a magic bullet, but they can be a great addition to your diet and exercise routine, offering some targeted anti-inflammatory backup.
Just remember, supplements are exactly that—supplementary. They work best as part of a healthy lifestyle. Before you start anything new, have a chat with your healthcare provider to make sure it's the right choice for you.
To help clear things up, here’s a quick summary of the most common questions people have about managing their joint health.
Quick Answers to Your Joint Health Questions
| Question | Quick Answer & Key Takeaway |
|---|---|
| Which supplements are best? | Fish Oil (Omega-3s) and Turmeric (Curcumin) have strong anti-inflammatory evidence. Vitamin D is also key for bone health and immune function. |
| Should I take Glucosamine? | It's a component of cartilage and might help slow deterioration, but the research is mixed. It's often combined with Chondroitin. |
| How do supplements work? | They provide concentrated compounds that can help block inflammatory pathways or support cartilage health, complementing the effects of a healthy diet. |
| Are they a replacement for diet? | Absolutely not. Think of them as helpers, not a cure-all. A healthy diet, exercise, and proper rest are still the foundation of good joint health. |
Always remember to talk with a professional before adding supplements, as they can interact with medications and may not be suitable for everyone.
How Often Should I Use a Topical Pain Reliever?
Topical analgesics are fantastic for managing flare-ups and the soreness that comes after a workout. Think of them as your go-to for immediate, targeted relief.
Use them when you need them most: the moment a flare-up begins, before an activity you know might cause some stiffness, or right after exercise to head off soreness. However, if you find yourself reaching for a topical multiple times every single day for the exact same problem, that's a sign. It means it's time to see a healthcare professional to figure out what's really going on underneath.
When you need fast, powerful, and reliable relief to keep you moving, MEDISTIK delivers. Our Canadian-made topical analgesics are designed to help you prime your body for activity, perform at your best, and restore comfort afterward. Take control of your joint and muscle pain by visiting our official website to find the right solution for you.
 - LIVRAISON GRATUITE POUR LES COMMANDES $50+
- LIVRAISON GRATUITE POUR LES COMMANDES $50+
 - LIVRAISON GRATUITE DÈS 40 $ D’ACHAT
- LIVRAISON GRATUITE DÈS 40 $ D’ACHAT


