Time to Heal Muscle Tear: A Guide to time to heal muscle tear Recovery

When you’re laid up with a muscle tear, the first question on your mind is almost always, "How long until I can get back to normal?" The truth is, there's no single answer—it all comes down to the severity of the injury.
Think of it like a frayed rope. A few loose strands are a relatively quick fix, but a rope snapped clean in two is a whole different ball game, demanding a much more intensive repair process. The time it takes to heal a muscle tear can range from 2-4 weeks for a mild strain to several months for a complete rupture.
Your Muscle Tear Healing Timeline Explained
Not all tears are created equal, which is why your recovery timeline is directly tied to the extent of the damage. To set realistic expectations, clinicians classify tears into three distinct grades.
Understanding these grades is the first step. Each one represents a different level of damage to the muscle fibres—kind of like the difference between a hairline crack in a wall and a total structural collapse.
Breaking Down the Grades of Injury
A muscle tear happens when the fibres making up your muscle are stretched past their limit or forced to contract too powerfully, causing them to break. The severity of that break dictates not just your healing time, but your entire rehab strategy.
- Grade 1 Tear: This is a mild strain. Only a small number of muscle fibres (less than 5%) are damaged. You’ll probably feel some tenderness and minor pain, but you should still have a full range of motion.
- Grade 2 Tear: This is a more significant, but still incomplete, tear. The pain will be more immediate, and you’ll likely see swelling and notice a real loss of strength. It means more extensive damage has occurred.
- Grade 3 Tear: The most severe injury—a complete rupture of the muscle. This usually causes intense pain, significant swelling, and a total loss of the muscle's function. In some cases, you might even see a visible gap or lump where the muscle has torn apart.
To give you a better idea of what to expect, we've put together a summary of the typical recovery periods for each grade.
Estimated Muscle Tear Healing Timelines by Grade
This table outlines the general timelines for recovery and a return to your usual activities, but remember that individual healing can vary.
| Tear Grade | Description | Estimated Healing Time | Typical Return to Activity |
|---|---|---|---|
| Grade 1 | Mild strain with minimal fibre damage (<5%). | 1-3 weeks | A few days to 2 weeks, with gradual progression. |
| Grade 2 | Moderate, partial tear with noticeable strength loss. | 4-8 weeks | 3-6 weeks, depending on the muscle and severity. |
| Grade 3 | Complete rupture of the muscle, often requiring surgery. | 3-6 months+ | 3-4 months post-op, with a full return often taking longer. |
These timelines are a guide. Factors like your age, overall health, and how well you stick to your rehab plan will all play a role in your final outcome.
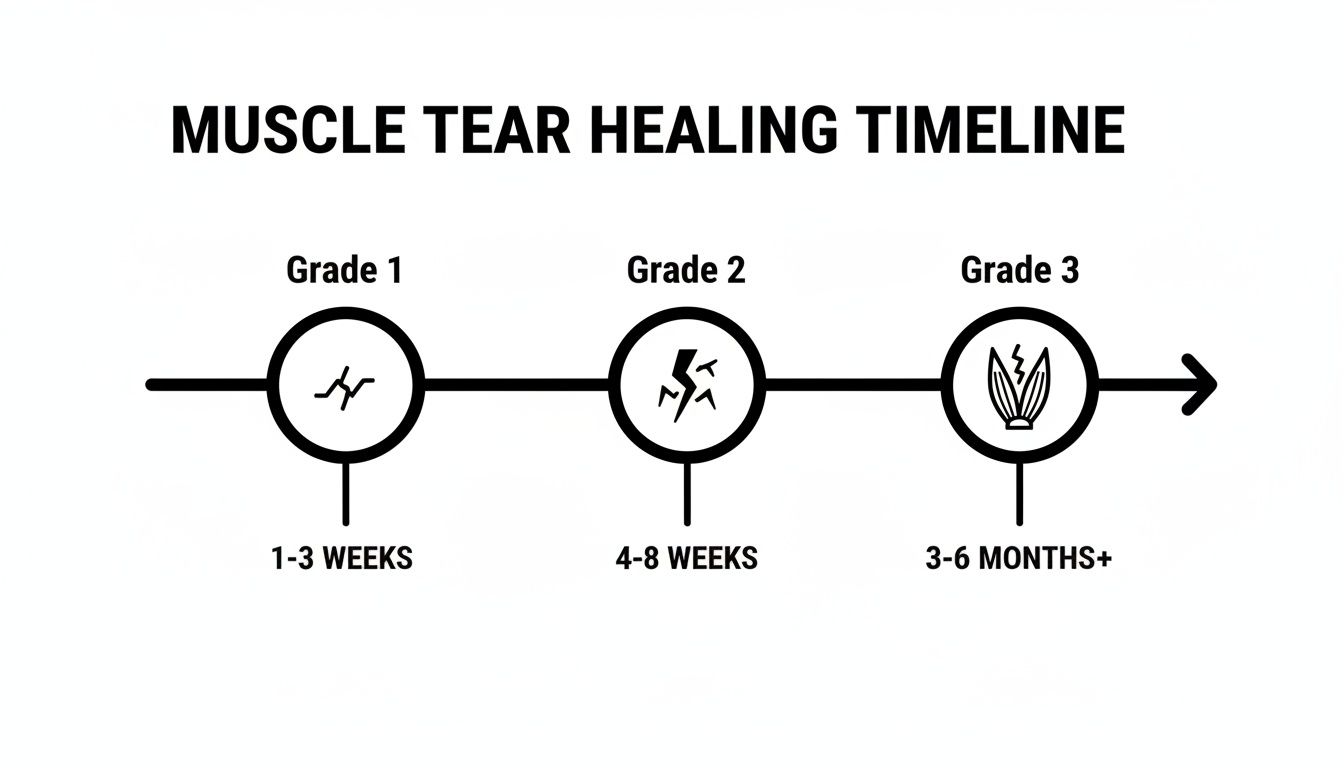
As you can see, the more severe the tear, the longer the road to recovery. It’s a journey from weeks to months, and each stage is critical.
The body's response to injury is a highly organized cascade of events. While timelines vary, the biological process of inflammation, repair, and remodelling remains constant. Rushing any of these phases is the most common cause of re-injury.
Each recovery phase builds on the last one. That’s why patience is just as crucial as physical therapy. Understanding this process helps you work with your healthcare provider to get back to your activities safely and effectively.
How Your Body Actually Repairs a Torn Muscle

When you tear a muscle, your body doesn't just patch it up; it kicks off an impressive, highly organized construction project to fix the damage. Getting a feel for this process helps explain why healing takes time and why patience isn't just a virtue—it's a biological necessity.
Think of it as a three-phase operation. The whole sequence is a finely tuned biological response that starts the second the injury happens, turning a moment of chaos into a structured repair job. Each phase blends into the next, creating a smooth transition from cleanup to rebuilding and, finally, to strengthening.
Phase 1: The Inflammatory Response
The first stage is inflammation, which is basically your body's emergency response team rushing to the scene. This phase usually lasts from one to three days. Right after the tear, damaged blood vessels leak blood into the area, which forms a hematoma—a collection of blood that acts like a temporary plug.
That initial swelling and pain you feel? That's the signal that the healing cascade is officially underway. Specialized cells arrive to clear out dead muscle fibres and debris, essentially demolishing the damaged parts of the structure to make way for the new build. It's uncomfortable, but this cleanup is an essential first step.
Phase 2: The Repair and Regeneration Phase
Once the site is cleared, the rebuilding can finally begin. This repair phase gets going around 24 to 48 hours after the injury and can last for several weeks, depending on how bad the tear is. This is where the real magic happens.
Satellite cells, which are like dormant muscle stem cells, are activated by the injury. They multiply and start forming new muscle fibres, called myofibres. These new fibres bridge the gap in the torn muscle, creating a fragile scaffold that will eventually become strong, functional tissue.
Think of this stage like weaving a new patch into a torn piece of fabric. The initial threads are weak and disorganized, but they create the necessary framework for a durable repair.
To support all this construction, your body needs a steady supply of building materials. Muscle repair relies heavily on structural proteins, and understanding the evidence-based benefits of collagen peptides can shed light on how these are used in recovery. Pushing the muscle too hard during this phase is like knocking over the scaffolding before the concrete has set—it just leads to re-injury and a much longer recovery time.
Phase 3: The Remodelling and Maturation Phase
The final stage is all about refinement. The remodelling phase starts not long after the repair work begins, but it can continue for a year or even longer. During this period, the newly formed, disorganized muscle fibres are gradually reorganized and made stronger.
This process is heavily influenced by the forces you put on the muscle. Gentle, progressive loading—the foundation of good physiotherapy—encourages the new fibres to align correctly, making them stronger and more resilient. The weak scar tissue that formed initially is slowly replaced with more robust, functional muscle tissue. This is exactly why a gradual return to activity is so important.
For temporary relief during this often-uncomfortable stage, many clinicians and athletes use topical analgesics like MEDISTIK. They can help manage the aches and pains that come with rehab, making it easier to stick with your program. Learning more about how pain is processed by the brain can also give you valuable insight into managing your discomfort effectively throughout the healing journey.
Factors That Influence Your Healing Speed
Ever wonder why one person’s muscle tear heals in a few weeks, while someone else with a similar injury is sidelined for months? The truth is, those healing timelines we talk about are really just educated guesses. The actual time to heal a muscle tear isn't set in stone; it’s shaped by a whole host of personal and biological factors.
Think of your body's repair process like a complex construction project. The success and speed of the job depend entirely on the quality of your tools, the efficiency of your supply chain, and the skill of your crew. A lot of different variables can either speed things up or grind the whole operation to a halt.
Key Variables in Your Recovery Equation
Several key elements play a massive role in how quickly you'll get back on your feet. Understanding what they are gives you the power to create the best possible environment for healing.
Some of the most critical variables include:
- Age: As we get older, our body's cellular repair mechanisms naturally slow down. Muscle regeneration isn’t as efficient, and collagen production declines, which can definitely extend recovery times.
- Nutrition: Healing is hard work for your body, and it needs a steady supply of fuel and raw materials. Not getting enough protein, vitamins (especially C and A), and minerals can create a major bottleneck, slowing down tissue repair.
- Sleep Quality: Your body does most of its heavy lifting for repairs while you sleep. Poor or insufficient sleep messes with the release of growth hormone, a key player in muscle regeneration and recovery.
Just these three factors alone can dramatically change your healing journey. But the list doesn't stop there.
Lifestyle and Injury-Specific Factors
Beyond the big three of age, diet, and sleep, other lifestyle choices and the specifics of the injury itself have a profound impact. Your circulatory system, for example, is the delivery service bringing oxygen and nutrients to the injury site. Any habit that gets in the way of that system will directly slow down your healing.
Things like smoking can constrict blood vessels, reducing blood flow and crippling that essential supply chain. Your overall health matters, too. Conditions like diabetes can impair circulation and compromise the body's ability to repair itself efficiently.
The specific muscle that was injured also plays a part. Larger muscles with a rich blood supply, like your quads, tend to heal faster than smaller muscles or those in areas with poorer circulation.
The location and blood supply of a torn muscle are critical. A muscle rich in blood vessels receives more "building materials" for repair, whereas areas with limited flow face a slower, more challenging reconstruction process.
Repetitive strain injuries (RSIs), which often involve micro-tears from overuse, are a perfect example of how the type of injury and age intersect. In Canada, RSIs once affected 1 in 10 adults, and the recovery timelines really highlight this connection. Younger individuals might regain strength in 10-21 days, while older adults can face months of recovery due to slower regeneration. You can explore more data on repetitive strain injury trends in Canada.
By taking control of the variables you can—like improving your diet, making sleep a priority, and managing your overall health—you actively support your body's natural healing abilities. You can also improve pain relief and recovery with targeted strategies that complement your body's efforts.
Your Roadmap to Muscle Tear Rehabilitation
A successful recovery is an active process, not a passive waiting game. Getting a handle on the time to heal a muscle tear means you need a structured plan—one that guides you from the initial shock of the injury all the way back to full function.
Think of it like climbing a mountain. You wouldn't just sprint to the summit; you’d set up base camps along the way. Each phase of your rehab is a new camp, giving you a chance to rest, adapt, and prepare for the next leg of the journey. This approach ensures you rebuild strength safely and effectively, dramatically lowering your risk of a setback.
To help visualize this journey, here's a quick look at the typical stages.
Rehabilitation Stages After a Muscle Tear
This table breaks down the goals, activities, and general timelines for each phase of recovery. Remember, these are guidelines—your personal timeline will depend on the severity of your injury and other individual factors.
| Rehab Phase | Primary Goal | Example Activities | Typical Duration |
|---|---|---|---|
| Acute Phase | Protect, manage pain & swelling | Rest, ice, gentle pain-free motion | 24–72 hours |
| Sub-Acute Phase | Restore range of motion, begin activation | Light stretching, isometrics, low-impact cardio | 3 days to several weeks |
| Strengthening Phase | Rebuild functional strength & power | Progressive resistance, sport-specific drills | Several weeks to months |
Let's dive deeper into what each of these phases actually involves on the ground.
The Acute Phase: Protection and Pain Control
The first phase, lasting from 24 to 72 hours, is all about damage control. Your only job right now is to protect the injured muscle from any more harm, manage the pain, and keep inflammation in check. This is absolutely not the time to "push through" anything; it's a period of smart, active rest.
During this stage, the focus is on gentle care:
- Protection: Steer clear of any activity that causes pain. Depending on the injury, this might mean using crutches for a bad leg strain or simply avoiding lifting with an arm injury.
- Pain Management: Applying ice for 15-20 minutes every few hours can help numb the area and calm down the swelling. To manage discomfort between icing, a topical analgesic like MEDISTIK can provide temporary relief right where you need it.
- Gentle Movement: Complete bed rest is rarely the answer. In fact, it can be counterproductive. Light, pain-free movements, like ankle pumps for a calf strain, encourage blood flow without putting any stress on the healing tissue.
The golden rule here is to listen to your body. Any sharp pain is a clear signal to stop and back off.
The Sub-Acute Phase: Restoring Movement
Once the initial sharp pain and swelling start to calm down, usually after a few days, you're stepping into the sub-acute phase. This stage can last for several weeks, and the main goal is to gently get your range of motion back and start waking up the injured muscle.
This is where the idea of ‘optimal loading’ becomes so important. It’s a delicate balancing act between doing too much and not doing enough. You need to apply just enough stress to the healing tissue to show the new fibres how to align correctly, but not so much that you re-injure it.
Activities in this phase often include:
- Gentle Stretching: Think slow, static stretches that you hold without any bouncing. The goal is to feel a light pull, never pain.
- Isometric Contractions: These are exercises where you tense the muscle without actually moving the joint. A great example is gently pushing your foot against a wall for a calf injury.
- Light Cardio: Low-impact activities are your friend here. Things like stationary cycling or swimming can keep your cardiovascular fitness up without stressing the injury.
Before you even think about moving on, you need to be able to achieve a full, pain-free range of motion in the affected joint. Hitting that milestone is your green light for the next, more demanding phase.
The Strengthening Phase: Rebuilding Functional Power
This final phase is all about getting your strength back and preparing the muscle to handle everything you throw at it—from daily life to your favourite sports. This stage can last anywhere from several weeks to many months, especially for more severe tears. The focus shifts from simple movements to progressive resistance training.
Your target is to regain strength that's at least 90% of your uninjured side before you consider a full return to your sport. This is where a physiotherapist's guidance is priceless; they can design a program that’s built specifically for you.
A key part of any solid rehab program is having a clear plan. If you're looking for structure, checking out some practical treatment plan templates can help you set and track your goals.
Rehabilitation isn't just about healing; it’s about remodelling. The exercises you do in this final phase are essentially teaching the new muscle tissue how to be strong, resilient, and ready for real-world forces.
Take rotator cuff tears, for example—a common muscle-tendon injury in Canada affecting an estimated 180,000 adults each year. Healing these tears follows a strict, phase-based timeline. While partial tears might heal in 3-6 months with good physio, a surgically repaired tear demands a much longer, carefully structured rehab process to get back to full function.
This structured roadmap, from that initial acute care all the way to functional strengthening, is your best bet for a successful recovery. Following these phases helps you understand how to best speed up your muscle strain recovery by working with your body’s natural healing process, not against it.
Knowing When to See a Professional
It can be tough to figure out what's normal pain and what's a serious problem during recovery. Some discomfort is just part of the healing game, but certain signs are your body’s way of screaming for help. Knowing the difference is key to getting back on your feet safely.
Think of it this way: a little background static on the radio is no big deal, but a blaring siren means you need to pull over immediately. The same goes for your body. Learning to spot these "sirens," or red flags, ensures you get professional help right when you need it, stopping a small issue from turning into a major setback.
Red Flags That Demand Medical Attention
As you manage your recovery at home, you need to be on high alert for specific warning signs. Blowing these off could seriously extend the time to heal your muscle tear or, worse, lead to it healing incorrectly. If you experience any of the following, it’s time to see a doctor or physiotherapist—no delays.
- A Loud ‘Pop’ or Snapping Sensation: If you clearly heard or felt a "pop" when the injury happened, it could signal a complete rupture (Grade 3 tear) or even damage to a nearby ligament or tendon.
- Visible Deformity in the Muscle: Take a look at the injured area. Do you see any strange lumps, gaps, or indentations? This is often a sign that the muscle has torn completely and pulled back, a situation that almost always needs medical intervention.
- Inability to Bear Weight or Move the Limb: If you can’t put any weight on the injured leg or are totally unable to move the affected arm, you're likely dealing with a severe injury that needs a professional diagnosis.
- Intense, Unrelenting Pain: Pain that is off the charts, doesn’t get better with rest and basic first aid, or actually gets worse over time is a huge red flag.
- Significant Swelling and Bruising: Rapid, widespread swelling or deep, dark bruising that shows up soon after the injury can point to serious internal bleeding and tissue damage.
These symptoms are a world away from the usual aches of a mild or moderate strain. They are clear signals that your injury likely needs a proper diagnosis, possibly with imaging like an ultrasound or MRI, and a formal treatment plan from a healthcare provider.
Trying to self-diagnose a severe injury is a gamble you don't want to take. A professional assessment gives you a clear diagnosis, rules out any nasty complications, and gets you started on the right recovery path from day one.
Putting off that professional visit when these signs are present can seriously compromise your healing. It’s always, always better to play it safe and get an expert opinion.
Effective Pain Management at Home
For less severe injuries that don't have any red flags, managing your discomfort at home is a huge part of the recovery equation. The goal isn't to just numb the pain, but to create an environment where your body can heal while you stay comfortable enough to do the gentle, therapeutic movements that will help you get better.
The classic P.O.L.I.C.E. protocol is a fantastic starting point for the first couple of days.
- Protection: Stop doing whatever causes pain. This prevents you from making the injury worse.
- Optimal Loading: As soon as you can tolerate it, introduce gentle, pain-free movement. This is crucial for stimulating healing.
- Ice: Apply an ice pack for 15-20 minutes every few hours. This helps dial down swelling and provides some numbing relief.
- Compression: Use an elastic bandage to gently wrap the area, which helps keep swelling in check.
- Elevation: Prop the injured limb up so it's higher than your heart. This helps drain away excess fluid.
Beyond these core steps, topical analgesics are a practical tool for managing localized pain. Products like MEDISTIK can be applied right on the sore spot to provide temporary relief from muscle aches. This targeted approach can make it much easier to stick with your rehab exercises, turning a painful chore into something far more manageable.
By understanding these boundaries, you can confidently take charge of your recovery and know exactly when it’s time to call in the pros.
Safely Returning to Your Favourite Activities

The real finish line in your recovery isn’t a date on the calendar—it’s when your body tells you it's ready. Pushing it too soon is a classic mistake that can undo weeks of careful healing and send you right back to square one. True readiness is so much more than just being pain-free while you're sitting on the couch.
Think of that healed muscle like a brand-new road. It might look solid on the surface, but that doesn't mean it’s ready for rush-hour traffic. It needs time to cure and prove it can handle the stress of heavy loads and high speeds. In the same way, your muscle has to pass a few crucial functional tests before it’s really cleared for action.
The Functional Readiness Checklist
Instead of just watching the weeks tick by, your focus should be on hitting specific, measurable milestones. These are the green lights that signal your tissue is strong enough to handle the demands of your sport or daily life. Before you even think about jumping back in, make sure you can confidently check off these boxes.
- Full, Pain-Free Range of Motion: You need to be able to move the injured limb through its entire range of motion without any pain, tightness, or second thoughts. It should feel just as smooth and easy as your uninjured side.
- Symmetrical Strength: Your injured side must be at least 90% as strong as your uninjured side. A physiotherapist can use objective tests to measure this, but you can get a pretty good idea by comparing movements like single-leg squats or calf raises.
- No Pain During Activity: This is a big one. You have to be able to perform movements specific to your sport without a hint of pain. For a runner, that means jogging, sprinting, and changing direction without a single twinge. For a weightlifter, it means hitting your lifts with good form and zero discomfort.
Meeting these benchmarks isn't optional. They're the foundation for a safe and lasting return, making sure your time to heal muscle tear leads to a full recovery, not another setback.
"A common pitfall is returning to sport when the pain is gone but functional strength is not restored. The muscle may feel fine during daily activities but lacks the capacity to absorb and produce the high forces required in sports, creating a perfect storm for re-injury."
Gradual Reintroduction Is Key
Once you’ve met all the readiness criteria, the last piece of the puzzle is a smart, gradual re-entry. You can't go from zero to one hundred. You need a structured plan to slowly reintroduce intensity and volume, giving that healed tissue a chance to adapt.
Start at a lower intensity, maybe around 50% of your usual effort, and for a shorter amount of time. If that feels good, you can begin to increase one variable at a time—either intensity, duration, or frequency—by about 10-15% each week. This methodical approach allows your body to get used to the load again, ensuring your comeback is not just successful, but permanent.
Common Questions About Healing Muscle Tears
Navigating the recovery process for a muscle tear can bring up a lot of questions. Getting clear, straightforward answers is key to making smart decisions and feeling confident about your healing journey.
Let's tackle some of the most common questions people have about the time to heal a muscle tear.
Should I Use Ice or Heat for a Muscle Tear?
This is the classic debate, and the right answer really depends on timing. For the first 48-72 hours after you pull a muscle, ice is your go-to. Applying a cold pack helps shrink the blood vessels, which is great for tamping down swelling, inflammation, and that immediate, throbbing pain.
Once you’re past that initial acute phase, you can switch over to heat. A warm compress or heating pad boosts blood flow to the injured spot. This helps relax tight, stiff muscles and can feel fantastic before you start any gentle rehab exercises.
Is Complete Bed Rest the Best Approach?
Not anymore. The old advice to stay completely still is outdated. While you definitely need to protect the muscle from more damage in the first few days, the modern approach centres around a concept called “optimal loading.”
This means introducing gentle, pain-free movement as soon as your body is ready for it. This light activity is crucial—it kickstarts the healing process, helps new muscle fibres line up properly, and stops the surrounding muscles from getting weak. The golden rule is to listen to your body and follow the lead of your physiotherapist.
Complete inactivity can actually lead to weaker scar tissue and drag out your recovery. The goal isn't to stop moving; it's to move smartly within pain-free limits to help your body do its repair work.
Can My Diet Help Speed Up the Healing Process?
Absolutely. What you eat plays a massive role in recovery. Think of it like giving your body’s internal construction crew the best possible materials to rebuild the damaged tissue.
Make sure you're getting enough protein, which provides the amino acid building blocks needed to create new muscle fibres. On top of that, foods rich in Vitamin C, Vitamin A, and zinc are critical for tissue repair and building collagen. And don't forget to stay well-hydrated—it's essential for keeping your cells functioning at their best.
For targeted, temporary relief from the aches and pains that come with recovery, trust MEDISTIK. Our powerful, Canadian-made topical analgesics can help you manage discomfort, making it easier to stay on track with your rehabilitation plan. Find the right product for your needs at https://medistik.com.
 - LIVRAISON GRATUITE POUR LES COMMANDES $50+
- LIVRAISON GRATUITE POUR LES COMMANDES $50+
 - LIVRAISON GRATUITE DÈS 40 $ D’ACHAT
- LIVRAISON GRATUITE DÈS 40 $ D’ACHAT


